Clinical Neurophysiology Tests of nerve conduction are used to identify damage to a nerve trunk as a result of pressure or transection or neuropathy, to trace the extent of regeneration of axons, to examine the extent of denervation or re-innervation of skeletal muscle using Electromyography, and to study the integrity of pathways in the CNS using Evoked Potentials |
|
Measurement of Conduction Velocity in Human Nerves |
|
Clinical Neurophysiology Tests include
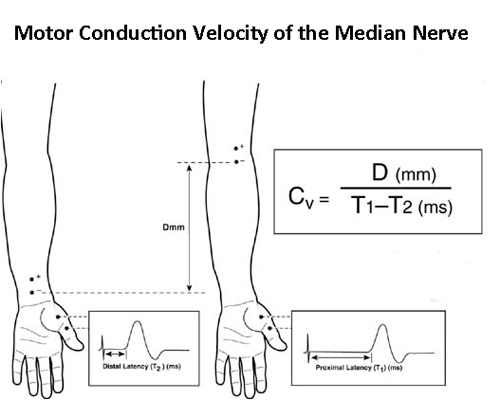
The first four in this list involve measurements of the conduction of action potentials in human nerves. Tests of nerve conduction velocity are relatively simple to perform and give an indication about the condition of the fastest sensory or motor fibres in the nerve. A commonly performed test to to examine the median nerve, as shown in the diagram. Electrical stimuli are applied through the skin overlying the median nerve in the distal forearm, and again at the elbow. Distal stimulation causes and action potential in the small muscles of the thumb, picked up by recording electrodes. The distal terminal latency is the time taken for the action potential to be conducted from nerve underlying the cathodal stimulating electrode to the nerve muscle junction plus the time taken to initiate the action potential in the muscles. Proximal stimulation initiates a similar series of events but the proximal latency also includes the time taken for the nerve action potential to be conducted the distance between the two stimulating electrodes (wrist and elbow)- which happens to be approximately a straight line. So the conduction velocity of the median nerve in the forearm can be calculated as shown. |
|
If the motor conduction velocity (CV) of the fastest fibres is >40 metres/second then the result is taken as normal. However, if the CV is <40 m/sec, the result is considered to be low and abnormal. It is important to be sure that a low result is not because the temperature of the limb nerve being tested is cold, because low temperature reduces the CV of peripheral nerves. If the temperature is normal, and the CV is <40 m/sec, then it can be concluded that the nerve is abnormal, possibly due to neuropathies associated with disorders such as diabetes. |
In the Carpal Tunnel Syndrome, pressure on the median nerve in the carpal tunnel causes the distal terminal latency to be greater than normal. However the proximal part of the median nerve in the forearm is unaffected by the compression, and the CV in the forearm is unaffected. Decompression of the carpal tunnel can return the distal terminal latency towards it normal value (<4.5 msec). |
Sensory Nerve CV in the median nerve. The conduction velocity of sensory axons can be examined by applying electrical stimuli to the nerve in the index or middle fingers (using ring electrodes), and recording a compound action potential from the median nerve in the wrist, using surface electrodes. The conduction velocity is the distance between the cathodal stimulating electrode and the onset of the action potential, divided by the latency- expressed in metres/second. Because no synapses are involved, the distance between stimulating and recording electrodes, is divided by the latency of the sensory action potential. This is probably the most sensitive index of peripheral nerve function. |
|
Other Nerve Compression Syndromes. The ulnar nerve can become compressed at the elbow (student's elbow - the 'funny bone') , and the radial nerve may be affected by fractures of the humerus in the region of the radial groove. In the lower limb, the common peroneal nerve can be compressed as it winds round the neck of the fibula, as a result of direct pressure of fracture of the bone. The motor nerve tests in the lower limb are focussed on the flexor digitorum brevis muscle, which is innervated by the common peroneal nerve. Loss of control of this muscle results in footdrop. Sensory testing in the lower limb examines the potentials generated in the sural nerve. |
Neuropathies are disorders of peripheral nerves that give rise to symptoms such as pins and needles (paraesthesiae), pain and numbness in the periphery of the limbs. Neuropathy can occur in metabolic disorders such as diabetes, or in nerve compression (say carpal tunnel syndrome),various infections and other aetiologies, and as a side effect of drugs. There may also be signs of denervation of muscle (muscle wasting and loss of power)
|